Children’s Healthcare of Atlanta is a leader in pediatric spine care. More kids, teens and young adults come to us for spine surgery than any other pediatric hospital in the country.* Not only do we rank among the best pediatric hospitals in the country for orthopedics, but we are also the only nationally ranked pediatric orthopedics program in Georgia.**

When it comes to your child’s spine surgery, experience and outcomes matter.
Children’s performs more spinal fusion surgeries than any other hospital dedicated to treating kids and teens, with some of the best spine surgery results in the nation. We are passionately dedicated to making sure your child has the best possible outcomes.
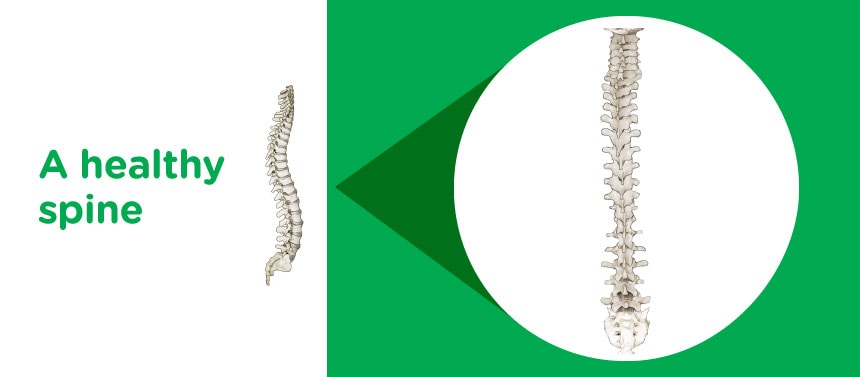
LEARN MOREThe spine withstands a lot of stress each day, making it a common site for an overuse injury, especially in growing children. Our team of pediatric spine specialists at Children’s Healthcare of Atlanta understands how the spine can change as your child or teen grows or if your child or teen is injured.
Spine problems in children can present at birth (known as congenital spine problems), develop over time as your child or teen grows, or be caused by an injury, such as a muscle strain from physical activity or improper weight lifting. Curvature of the spine (scoliosis) can occur in otherwise healthy children for no apparent reason, although the tendency can run in the family. Heavy backpacks can also be a source of back pain, as suggested weight limits are no more than 15% of a child’s or teen’s body weight.
If an issue arises or back pain continues in your child or teen, we recommend treatment by someone who is specially trained in caring for the pediatric spine. At Children’s, our specialists help care for, diagnose and treat spine problems in children of all ages, from birth to 18.
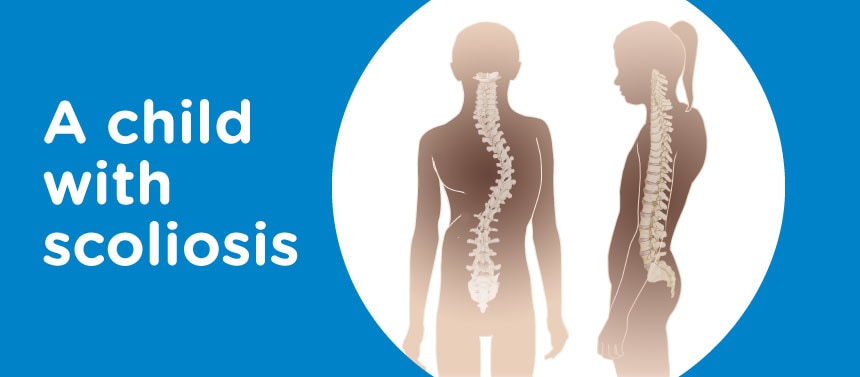
Scoliosis is a lateral, or sideways, curvature of the spine greater than 10 degrees. This also includes types of neuromuscular scoliosis like spina bifida, cerebral palsy, spinal muscular atrophy (SMA) and muscular dystrophy.
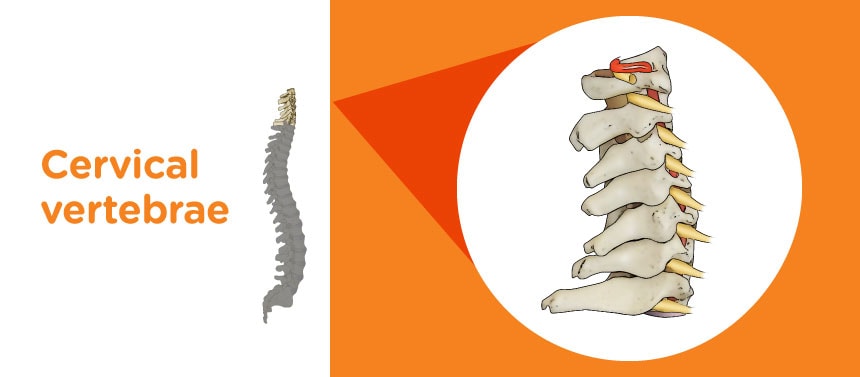
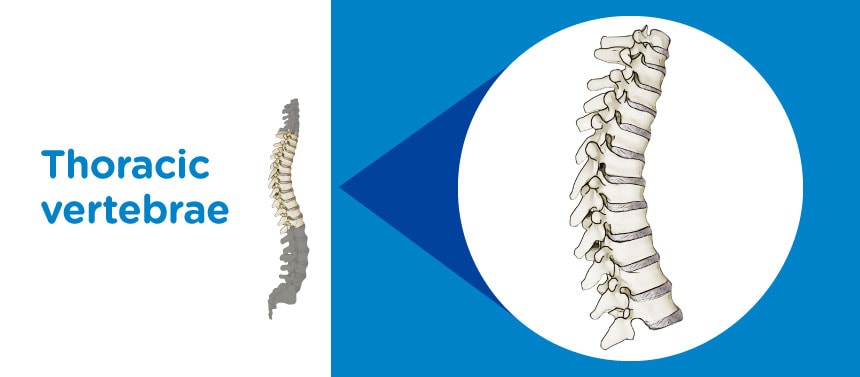
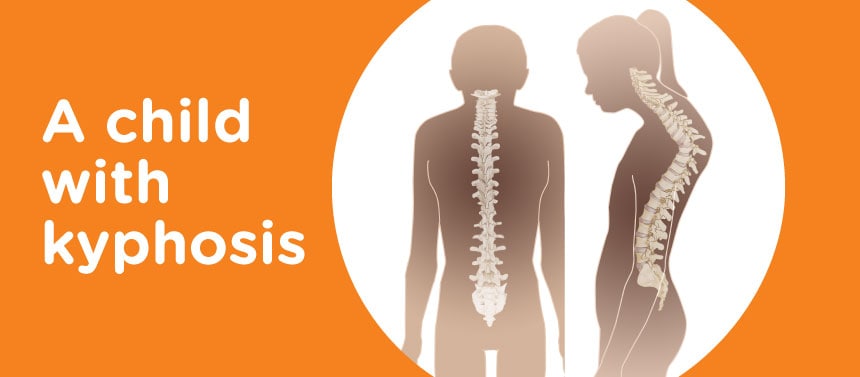
Kyphosis refers to the rounding of the upper back in a C-shaped curve, or a hunched back. Kyphosis most commonly affects the thoracic spine (upper and middle back) but can also involve the cervical (neck) and lumbar (lower back) portions. The two most common types of kyphosis are Scheuermann’s kyphosis and postural kyphosis. Kyphosis may develop because of:
- Metabolic problems
- Neuromuscular conditions
- Spina bifida
- Osteoporotic fractures
- Traumatic injuries
- Slippage of vertebral disc
The symptoms of kyphosis may vary based on how severe they are. They may range from a minor change in the shape or appearance of the back to more severe nerve problems and long-lasting back pain. There may be weakness in the legs because of the pressure that is put on the spinal cord and nerve from the spinal curvature. Trouble breathing may also develop because of pressure over the lungs. Evaluations and diagnostic tests may include:
- A complete medical history
- A physical examination by a doctor to evaluate spine movement, muscle strength, and sensation, to help the doctor make a proper diagnosis and also rule out other similar conditions
- Some diagnostic tests, such as X-rays, a magnetic resonance imaging (MRI) scan and a computed tomography (CT) scan, to see the structure of the spine and measure the curve
Kyphosis has several treatment choices that range from medicines to exercises including physical therapy and casts and support braces. Spine surgery may also be considered in some cases.
In cases where osteoporosis causes kyphosis, it’s recommended that your child do the following to slow down the condition’s progress:
- Take vitamin D and calcium supplements.
- Use hormone replacement therapy.
- Exercise regularly.
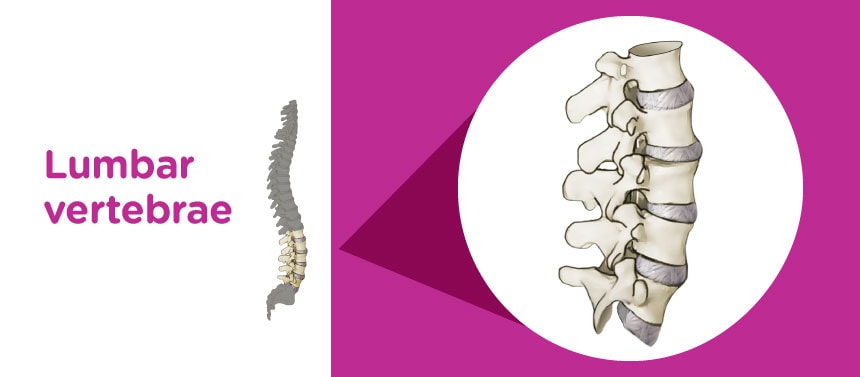
Spondylolysis, also known as stress fractures, is a defect in the spine at a part of the bone known as the pars interarticularis. This pars region connects the front part of the backbone (vertebral body), which houses the spinal cord and nerves, to the back part of the backbone (posterior elements).
Spondylolysis is caused by genetics, overuse or repeated injuries, or a combination of the three. Children at highest risk to develop these defects are those who join in sports that require children to repeatedly arch their backs. Those sports include gymnastics, cheerleading, weight lifting and football.
Many children are symptom-free, and the condition is often overlooked. However, when spondylolysis has symptoms, it is typically lower back pain, which is made worse because of arching the back. In rare cases, your child could feel pain that goes down the legs. The pain is typically severe enough that your child may not want to join in a sport.
Spondylolisthesis, or a slipped vertebra, is commonly associated with spondylolysis. Spondylolisthesis typically occurs when someone has spondylolysis, and then as a result, one bone slips forward in relation to another.
These two conditions are the most common causes of chronic back pain in children.
At your appointment, your child’s doctor will look for signs of stress fractures by:
- Taking a complete medical history.
- Doing a physical examination.
- Getting an X-ray of the lower back.
Sometimes a computed tomography (CT) scan or a magnetic resonance imaging (MRI) scan might be used to look for very small fractures, to rule out other possible causes of pain and to plan treatment options.
A moderate approach will often work to treat spondylolysis, including rest, medication and physical therapy.
Treatment is intended to reduce pain and swelling, which usually allows the fracture to heal. In some cases, a back brace may be worn for a short time to take the pressure off the lower back. If your child’s pain continues, he or she may need surgery.
Trauma injuries to the spine may include spinal fractures and post-traumatic spine problems.
Acute spine injuries happen suddenly. This can be cause from things such as a car accident or a fall.
Burst fractures—thoracic or lumbar spine fractures—generally result from a high-energy impact, such as a car crash, fall from a height or contact sports, that forcefully smashes the spine. The energy of the injury causes the vertebrae to fracture, or burst, into multiple pieces, and the injured vertebrae lose height, which can lead to instability and a deformity and/or injury to the spinal cord.
X-rays of the spine, including upright or standing, are necessary to determine if the spine is stable. A CT or computerized axial tomography (CAT) scan and/or an MRI may be required for a better view of the injury.
Generally, stable burst fractures are treated with braces and pain medication. However, unstable fractures require surgical stabilization to protect the spinal cord from injury and the spine from future deformity. Any fracture-associated spinal cord compression will need surgery to decompress the cord.
Chronic spine injuries are spine injuries that are ongoing. This can be caused by muscle strains and overuse, but constant pain could be a sign of something more serious.
Up to 50% of teens will experience back pain before the age of 20. Most back pain will resolve without treatment. In children age 10 and under, back pain is extremely uncommon unless there is a specific injury. In fact, the most common cause is constipation. If your child or teen has ongoing pain, consider setting up an appointment to be seen by a doctor.
Common sources of back pain in children and adolescents include:
- Overuse/muscle strains
- Stress fractures (spondylolysis)
- Scheuermann’s kyphosis
- Herniated disc
- Backpacks
Childhood back pain can be caused by a variety of issues ranging from normal growing pains to activity-related injuries requiring urgent treatment. Your child needs immediate medical attention if he has any of these symptoms:
- Constant back pain
- Pain that’s only in one specific area
- Pain that requires pain medication
- Pain that limits activities
- Pain associated with fevers, chills and weight loss
In the adolescent age group, back pain is very common and is usually concentrated across the middle of the lower back—and may be noticed especially when sitting or standing for long time periods. You may also notice that your child slouches more often and insists it hurts to sit up straight.
It’s normal for a teen to experience aches right after a growth spurt—muscles typically grow strong before they grow long—but these aches rarely require pain medication or limit activity.
In order to stop the backache, your child may need to build up back and core strength, and a short course of physical therapy may be helpful.
Back pain is an extremely broad topic and may or may not be due to the back itself. Your child’s doctor will complete a physical examination and ask several questions to determine the cause and location of the pain. If necessary, X-rays will be ordered during the initial visit, and then imaging tests and blood work may be recommended at subsequent visits if the cause is still not clear.
Tumors and infections in the bone can include aneurysmal bone cysts, osteoblastoma (sarcoma), histiocytosis, malignant tumors and osteomyelitis.
A unicameral bone cyst, also known as a simple bone cyst, is a benign (not cancerous) bone tumor. These tumors are most commonly found near the shoulder and hip joints. They often go away without treatment after your child has completed the growth cycle.
Bone and joint infections (osteomyelitis and septic arthritis) occur much more commonly in children than in adults, with the majority of cases occurring in children under the age of 5. Our team understands these infections.
Vertebrae problems, or problems with the discs of the spine, can include degenerative disc disease, herniated discs or other disc disorders.
In recent years, disc herniation in children has become more common. A herniated disc develops when one of the discs between the bones (vertebrae) of the spine moves out of position and presses on adjacent nerves, causing pain in the back, pain in one or both legs and numbness, tingling or weakness in one or both legs. These discs are cushions that have a soft center and a hard outside. If the hard part of the disc cracks and the soft part is exposed, it is called a hernia. A herniated disc can also be called a “pinched nerve” or “bulging disc.”
Deformities of the spine or chest can be associated with other conditions, such as Prader-Willi syndrome, Jeune syndrome, congenital rib fusions, Down syndrome, Marfan syndrome, Ehlers-Danlos syndrome, Rett syndrome, Friedreich’s ataxia, osteogenesis imperfecta and achondroplasia.
Our spine specialists treats thousands of growing spines each year, so we understand what symptoms to look for and how to diagnose babies, kids and teens.
We work closely with other pediatric specialists to review diagnostic tests that may include:
- A thorough medical history and physical examination
- Routine radiographs with low-dose imaging, such as X-rays
- An MRI
- A low-dose CT scan
- An ultrasound or a bone scan
Our pediatric radiologists receive advanced training, as well as following guidelines and protocols like dose-reducing technology that allows us to cut CT and X-ray radiation exposure by more than 50% compared to adult facilities.
Our spine team is specially trained to develop treatment plans for children and teens of all ages and to monitor patients over time so they have better results as they continue growing.
Treatment options for pediatric spine conditions and injuries may include:
- Medication
- Casting or bracing (orthotics)
- Pain management
- Physical therapy and sports physical therapy
- Spinal rest (your child may need to stop some activities while healing)
- Spine surgery
Spine bracing
Spine bracing is used to help prevent curves in the spine from getting larger as your child grows. Generally, curves less than 20 degrees don’t require treatment, since most do not worsen, but children whose curve is larger than 20 degrees are candidates for either part-time bracing (approximately 16 hours a day) or night bracing. Braces do not make curves go away but may prevent the curve in your child’s spine from worsening.
For some children, bracing may not be the best treatment. This may be because of the spine’s curve type, spine stiffness, the spine’s remaining growth, other medical problems or previous surgeries. These are each considered to help our specialists determine which treatment is best for your child’s spine.

Our team is very experienced in a variety of advanced bracing techniques
Our orthotics and prosthetics team uses some of the latest in casting and bracing techniques. We fit more than 600 spinal devices for our patients each year.
Learn MoreSpine casting
Serial casting is a special technique that does not require an incision but does require anesthesia to apply a casting technique called “elongation, derotation, flexion” (EDF) is used to slowly reduce the size of the curve in your child’s spine over several months. This is usually an outpatient procedure. EDF casting can result in complete correction of the curve, or at least allow for bracing of a smaller curve. This procedure is typically reserved for preadolescent children under 10 years old.
Spine surgery
If your child, teen or young adult needs surgery, our doctors are on the forefront of spine surgery innovations. We treat more spine patients than any other program in the country, and offer advanced procedures like halo-gravity traction to ensure each child has access to the right treatments for them. Our dedicated surgical team sets the standard for quality and safety in pediatric spine surgery. To coordinate care, we utilize clinical practice guidelines that dictate a high standard of care and help our patients get back to being kids more quickly. Our surgical team includes surgeons, anesthesiologists, nurses and operating room techs, each with a dedicated role to safeguarding the patient journey.
Children’s has some of the best spine surgery results in the nation. Our team continuously refines the surgical processes, including before, during and after surgery. Compared to other pediatric hospitals, our patients:
- Are in great company: Children’s performs more spine surgeries than any other pediatric hospital in the U.S.*
- Recover more quickly: Our team works diligently to help make sure patients can go home as soon as possible after surgery. In fact, Children’s has a shorter average length of stay for spine procedures than most children’s hospitals in the country.*
- Experience fewer complications: Children’s spine patients report fewer problems following surgery and fewer emergency department visits while recovering from surgery.*
What types of spine surgery are there?
The type of spine surgery recommended for your child or teen depends on several things, including your child’s or teen’s unique condition, previous treatments and whether he or she has a lot of growth still remaining. Larger curves (greater than 40 degrees) in younger children can be challenging to manage, but our skilled team will carefully evaluate all treatment options and may recommend an advanced procedure like halo-gravity traction prior to surgery to support the best surgical outcome for your child.
We want our patients and families to have the best possible experience during their spine surgery journey.
Concierge services
Our dedicated concierge team includes a spine program manager who helps coordinate a patient’s experience by providing complete follow-up care and helping make sure families have the information and resources they need before, during and after care. The spine program manager also serves as a single point of contact for your child and his or her primary care provider.
The spine program manager will help coordinate care by:
- Providing information about lodging and key contacts for those who live outside metro Atlanta.
- Arranging travel accommodations to Atlanta and transportation while in Atlanta.
- Helping families navigate the hospitals and escorting them as needed.
- Assisting with the hospital intake process and clinic visits.
- Writing treatment plans for your child’s or teen’s referring provider.
- Assisting in arranging the use of durable medical equipment after your child or teen is released from the hospital.
- Coordinating interpretation services.
- Coordinating financial planning with insurance companies.
- Following up with you after your child’s or teen’s procedure or visit.
- Communicating and coordinating requests for your child’s or teen’s referring provider.
Contact concierge services at 404-255-1933.
The Scoliosis and Spine Program at Children’s is led by Nicholas D. Fletcher, MD, Medical Director, and Joshua Murphy, MD, Medical Director, Spine Quality and Outcomes.
Members of the Children’s Orthopedics Program collaborate on patient care. We work closely with specialists from across the country and around the world to help establish best practices for pediatric spine care, and we are on the forefront of advanced technologies. Doctors in our Scoliosis and Spine Program also collaborate with neurosurgeons, anesthesiologists, physiatrists and other specially-trained physicians to care for kids, teens and young adults with complex neurological spine disorders, like certain types of scoliosis. Our Orthopedics Program and Neurology and Neurosurgery Program are both nationally ranked, combining experience and specialized training from two of the top programs in the Southeast to treat chronic back and neck pain, herniated discs, spinal cord tumors and degeneration and other conditions in patients from 0 to 18 years old.
Children’s Physician Group–Orthopaedics and Sports Medicine
Orthopedic surgeons:
- Jed Axelrod, MD
- Robert W. Bruce Jr., MD
- Dennis P. Devito, MD
- Jorge A. Fabregas, MD
- Nicholas D. Fletcher, MD
- Joshua Murphy, MD
- Michael L. Schmitz, MD

Athens Orthopaedics
1181 Langford Drive, Building 200, Suite 101
Watkinsville, GA 30677
Buford Orthopaedics
2914 Vinson Court
Buford, GA 30518
Center for Advanced Pediatrics
2174 North Druid Hills Road NE
Atlanta, GA 30329
Children’s at Cherokee
1558 Riverstone Parkway, Suite 100
Canton, GA 30114
Children’s at Duluth
2270 Duluth Highway 120
Duluth, GA 30097-4010
Children’s at Fayette
1265 Highway 54 W, Suite 200
Fayetteville, GA 30214-4526
Children’s at Forsyth
410 Peachtree Parkway, The Collection at Forsyth
Cumming, GA 30041-7407
Children’s at Hamilton Creek
2240 Hamilton Creek Parkway, Suite 600
Dacula, GA 30019
Children’s at Hudson Bridge–Orthopaedics and Sports Medicine
1492 Hudson Bridge Road
Stockbridge, GA 30281
Children’s at Meridian Mark
5445 Meridian Mark Road NE
Atlanta, GA 30342-4755
Children’s at Old Milton Parkway
3300 Old Milton Parkway
Alpharetta, GA 30005
Children’s at Town Center Outpatient Care Center
605 Big Shanty Road NW
Kennesaw, GA 30144-3646
Children’s Orthopedics and Sports Medicine – Douglasville
Opening September 6, 2022
6095 Professional Parkway,
First Floor, Suite 101B
Douglasville, GA 30134
Macon
4660 Riverside Park Blvd.
Macon, GA 31210
*Pediatric Health Information System (2023), as prepared by the Children’s Hospital Association. This report compares clinical data annually for more than 52 pediatric hospitals in the U.S.
**No. 10 on the U.S. News & World Report “Best Children’s Hospitals” list for 2023-24.
Contact Us 404-255-1933