Atlanta: Home to a Top Pediatric Research Program
About Our Research Program
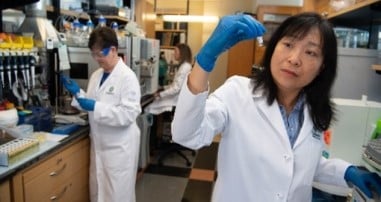
Led by our Pediatrician-in-Chief Shari Barkin, MD, and Chief Research Officer Kristy Murray, DVM, PhD, the Children's research program, in partnership with Emory University School of Medicine, has ranked in the top five for National Institutes of Health (NIH) funding for nearly a decade. Because of this transformative partnership, Children’s boasts a vast research ecosystem across a variety of pediatric disciplines. In addition to Emory, our other Atlanta-based research collaborations include the Children’s Healthcare of Atlanta Pediatric Technology Center (PTC) at Georgia Tech, Morehouse School of Medicine and the U.S. Centers for Disease Control and Prevention (CDC). Through these unique relationships and more, Children’s is advancing lifesaving treatments to make kids better today and healthier tomorrow as well as training the next generation of physician-scientists. Watch some of the incredible stories of our research breakthroughs.
Research is also conducted across our 11 specialty areas ranked by U.S. News & World Report’s list of “Best Children’s Hospitals,” for excellence in outcomes, program structure and national reputation. Learn more about each of these research programs below.

Marcus Center for Cellular Therapy
The Marcus Center for Cellular Therapy offers cell and gene therapy for patients with a variety of diseases—not just cancer. Therapies are manufactured in-house at the center’s good manufacturing practices (GMP) lab and are delivered directly to patients.
Life Changing Impact of Children's Research
-
Participating in CF Research Transforms James' Life
James is one of only 33 people in the world with a rare CF mutation. After joining a clinical trial for a new treatment, James takes just three pills a day instead of 60.
-
The Marcus Center for Cellular Therapy and Kyles Dream
Thanks to a significant grant from the late Bernie Marcus and The Marcus Foundation, the center shortens wait times for delivery of cell and gene therapies to patients like Kyle.

Emory University, Our Primary Research and Academic Partner
Children’s and Emory University School of Medicine partner together on clinical trials, residencies and fellowships. More than 500 physicians hold titles at both institutions. Our research program has ranked in the top five nationally for National Institutes of Health (NIH) funding for a decade.
Learn About EmoryResearch by the Numbers
In 2025, Children's reached a number of research milestones, including those below.

Clinical Trials
Children’s is involved in more than 1,200 clinical trials locally, nationally and abroad. Find or join one of our trials. Narrow your search by including a specific condition or disease.
Find Our Trials
View Our Research and Education Reports

Physician/PhD Careers with Children's
There’s never been a better time to be at Children’s. We’re growing to help ensure we can provide advanced pediatric care—not just today, but for generations to come.
learn more