Heart Research
At the Children’s Healthcare of Atlanta Heart Center, we’re committed to improving prevention and treatment of heart disease in children so that they can lead healthier lives. Our researchers are seeking innovative ways to improve the lives of children born with congenital heart disease (CHD) as they reach school age to prevent and treat the effects it has on children and teens.
We treat more than 40,000 heart patients each year and work closely with neighboring academic partners, including Emory University School of Medicine and Georgia Institute of Technology, to develop pediatric heart research. These research partnerships, combined with our experience in treating congenital heart defects in children of all ages, have allowed us to become a national leader in heart disease research.
The Emory University and Children’s Pediatric Research Unit is one of nine core sites in the Pediatric Heart Network (PHN). Created and funded by the National Heart, Lung and Blood Institute—part of the National Institutes of Health (NIH)—the PHN is a collaboration of clinical sites and a data coordinating center that conducts research studies in children with heart disease.
Learn more about the Pediatric Heart Network.
The Children’s Heart Research and Outcomes Center (HeRO) is a research partnership between Children’s, Emory University and the Walter H. Coulter Department of Biomedical Engineering at the Georgia Tech College of Engineering. HeRO seeks to reduce the morbidity of pediatric heart disease and leads the transformation of focused cardiac research into innovative therapies for young patients. Some of the primary focus areas of this research include regenerative and nanomedicine technologies, cardiac development, cardiac outcomes, cardiac devices and neurodevelopmental studies.
HeRO strives to create the next generation of pediatric-specific therapies through cutting-edge research using nanotechnology and stem cells, resulting in a better understanding of normal and abnormal cardiovascular development. Our researchers look at the whole picture and consider what will happen to these children from a neurodevelopmental standpoint as they age. By studying daily function and long-term outcomes, HeRO aims to have a better understanding of how to help children with heart disease regain normal function. This approach blends fundamental basic science with translational and clinical medicine to improve the quality of life for children with congenital heart disease.

Children’s Leads One of the First Pediatric Heart Studies Looking at Blood Oxygen Levels and Race
Children’s Cardiologists Alaa Aljiffry, MD, and Marco Mills, MD, led a study in African American and white infants undergoing heart surgery to determine differences in arterial oxygen saturation. Findings showed greater differences during the preoperative period, higher than adult reports, regardless of race.
Read the Study
Children’s Cardiologist Publishes COVID-19 Vaccination and Myocarditis Research
Dr. Matthew Oster, pediatric cardiologist at the Children’s Heart Center, uses data collected by the U.S. Centers for Disease Control and Prevention (CDC) to study rates of myocarditis after mRNA-based COVID-19 vaccination in more than 190 million children and adults.
read the studySupporting the Latest Pediatric Heart Research
-
Patient Family Gives Back After Tetralogy of Fallot Surgery
At the Children’s Heart Center, surgeons performed a surgery to repair Dax’s heart when he was 5 months old. Now, his family pays it forward by supporting heart research.
Latest News from the Children's Heart Center
Cardiology 2026: 29th Update on Pediatric and Congenital Cardiovascular Disease
Paul Chai, MD
Friday, Feb. 27:
12:00pm | Strategies and Techniques for Surgical Treatment of Coronary Abnormalities… and A Word About the Coronary Sinus
Saturday, Feb. 28:
12:30 pm | The Yasui Operation: For Whom and How? All at Once or Staged?
At the Children’s Heart Center, we work closely with other pediatric heart centers across the country and use innovative technology to develop treatments for pediatric heart disease so that our patients can live healthy lives. Our pediatric heart research collaborations include:
Congenital Cardiac Research Collaborative (CCRC)
The Children’s Heart Center is home to the CCRC, which is a multicenter research consortium studying outcomes following catheterizations, and surgical and nonsurgical interventions. Nine other centers are involved. Since founding the CCRC in 2014, our team has received numerous awards and authored many publications.
Pediatric Heart Network
As one of 10 core sites in this NIH multicenter collaboration, we are working to define best practices for treating pediatric heart disease. We are leading a network investigation of collaborative learning to improve postoperative management.
Children’s Heart Research and Outcomes Center (HeRO)
HeRO is a dedicated research center focused on problems associated with pediatric heart diseases. The center promotes partnership of scientists with pediatric cardiologists and cardiothoracic (CT) surgeons at the Heart Center to align basic research with patient-oriented studies aiming to improve the lives of children with heart disease.
Cardiovascular Imaging Research Core (CIRC)
We provide noninvasive imaging services, including electrocardiogram (ECG), echocardiography, stress test, stress echocardiography and cardiac MRI, for cardiovascular research involving infants, children and adolescents. The CIRC has dedicated space, equipment and staff to provide quality cardiovascular imaging data that is systematically collected.
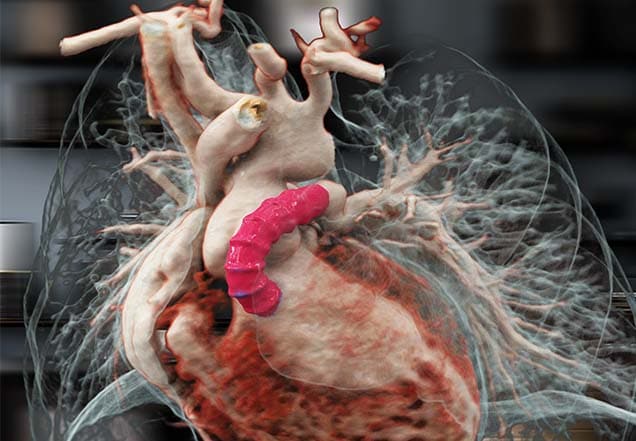
Cardiac imaging
We provide investigators across the country with advanced pediatric cardiovascular imaging services and research support. In collaboration with Georgia Tech, our CT surgeons use imaging to reconstruct a heart in 3D before surgery. This enables surgeons to better plan an operation based on the unique features of a patient’s heart.
Genetics and Precision Medicine: Heritable Thoracic Aortic Disease
Heritable thoracic aortic disease (HTAD) can have life-threatening consequences if not diagnosed early. Affected individuals and at-risk family members benefit from both cardiology and genetic evaluations, including genetic testing. Important information can be obtained through family history, medical history, and genetic testing to help guide management and assess risk. A genetic diagnosis can guide cardiovascular management (type and frequency of vascular imaging, timing of surgical intervention), risk assessment for arterial aneurysm/dissection, evaluation of nonvascular features, and familial testing.
A Novel Anisotropic Failure Criterion with Dispersed Fiber Orientations for Aortic Tissues
Accurate failure criteria play a fundamental role in biomechanical analyses of aortic wall rupture and dissection. Experimental investigations have demonstrated a significant difference of aortic wall strengths in the circumferential and axial directions. Therefore, the isotropic von Mises stress and maximum principal stress, commonly used in computational analysis of the aortic wall, are inadequate for modeling of anisotropic failure properties. In this study, we propose a novel stress-based anisotropic failure criterion with dispersed fiber orientations. In the new failure criterion, the overall failure metric is computed by using angular integration (AI) of failure metrics in all directions. Affine rotations of fiber orientations due to finite deformation are taken into account in an anisotropic hyperelastic constitutive model. To examine fitting capability of the failure criterion, a set of off-axis uniaxial tension tests were performed on aortic tissues of four porcine individuals and 18 human ascending thoracic aortic aneurysm (ATAA) patients. The dispersed fiber failure criterion demonstrates a good fitting capability with the off-axis testing data. Under simulated biaxial stress conditions, the dispersed fiber failure criterion predicts a smaller failure envelope comparing to those predicted by the traditional anisotropic criteria without fiber dispersion, which highlights the potentially important role of fiber dispersion in the failure of the aortic wall. Our results suggest that the deformation-dependent fiber orientations need to be considered when wall strength determined from uniaxial tests are used for in vivo biomechanical analysis. More investigations are needed to determine biaxial failure properties of the aortic wall.
Bicuspid Aortic Valve and Sports Clearance
Biomechanical properties of the thoracic aorta in Marfan patients
Marfan syndrome (MFS), a genetic disorder of the connective tissue, has been strongly linked to dilation of the thoracic aorta, among other cardiovascular complications. As a result, MFS patients frequently suffer from aortic dissection and rupture, contributing to the high rate of mortality and morbidity among MFS patients. Despite the significant effort devoted to the investigation of mechanical and structural properties of aneurysmal tissue, studies on Marfan aneurysmal biomechanics are scarce. Ex vivo mechanical characterization of MFS aneurysmal tissue can provide a better insight into tissue strength outside the physiologic loading range and serve as a basis for improved risk assessment and failure prediction.
Accurate identification of in vivo nonlinear, anisotropic mechanical properties of the aortic wall of individual patients remains to be one of the critical challenges in the field of cardiovascular biomechanics. Since only the physiologically loaded states of the aorta are given from in vivo clinical images, inverse approaches, which take into account of the unloaded configuration, are needed for in vivo material parameter identification. Existing inverse methods are computationally expensive, which take days to weeks to complete for a single patient, inhibiting fast feedback for clinicians. Moreover, the current inverse methods have only been evaluated using synthetic data. In this study, we improved our recently developed multi-resolution direct search (MRDS) approach and the computation time cost was reduced to 1~2 hours. Using the improved MRDS approach, we estimated in vivo aortic tissue elastic properties of two ascending thoracic aortic aneurysm (ATAA) patients from pre-operative gated CT scans. For comparison, corresponding surgically-resected aortic wall tissue samples were obtained and subjected to planar biaxial tests. Relatively close matches were achieved for the in vivo-identified and ex vivo-fitted stress-stretch responses. It is hoped that further development of this inverse approach can enable an accurate identification of the in vivo material parameters from in vivo image data.
Smooth muscle dysfunction syndrome (SMDS) due to heterozygous ACTA2 arginine 179 alterations is characterized by patent ductus arteriosus, vasculopathy (aneurysm and occlusive lesions), pulmonary arterial hypertension, and other complications in smooth muscle-dependent organs. We sought to define the clinical history of SMDS to develop recommendations for evaluation and management.Do HCN4 Variants Predispose to Thoracic Aortic Aneurysms and Dissections?
Hyperpolarization-activated cyclic nucleotide-gated channel 4 plays a key role in the generation of sinus rate and rhythm. Mutations in the corresponding gene, HCN4, are associated with sinus bradycardia, left ventricular noncompaction cardiomyopathy (LVNC), and mitral valve disease (MIM#613123-Brugada Syndrome 8 and MIM#163800-Sick Sinus Syndrome 2). More recently, Vermeer et al1 reported HCN4 variants that co-segregated with ascending aortic dilatation, LVNC and sinus bradycardia in 8 families, expanding the phenotype of HCN4 rare variants to include thoracic aortic disease (TAD). Subsequently, Arbustini et al2 questioned the association of thoracic aortic aneurysms with HCN4 mutations because numerous rare variants were identified in HCN4 in cases with TAD and other conditions, but none segregated with disease in families; and these rare variants were identified in cases with pathogenic and other rare variants in cardiovascular disease genes.
Mutations in the EFEMP2 (alias FBLN4) gene, which encodes the extracellular matrix protein fibulin-4, lead to severe aortopathy with aneurysm formation and vascular tortuosity. The disease phenotype, termed autosomal recessive cutis laxa type 1B (ARCL 1B), is rare among heritable connective tissue diseases but becomes more likely when noting family consanguinity and loose, inelastic skin in the patient. Our patient presented with an intercurrent illness exacerbating upper airway obstruction due to compression from a large aortic aneurysm. Genetic testing eventually revealed the causative mutation. She was initially treated with an angiotensin II receptor blocker and beta-blocker and eventually underwent total thoracic aortic replacement via a two-stage elephant trunk-type procedure. She recovered well and is currently asymptomatic but will require lifetime follow-up due to residual vascular tortuosity and aneurysm risk.
Atenolol versus Losartan in children and young adults with Marfan's syndrome.
Aortic-root dissection is the leading cause of death in Marfan's syndrome. Studies suggest that with regard to slowing aortic-root enlargement, losartan may be more effective than beta-blockers, the current standard therapy in most centers.
Patients with the Marfan syndrome (MFS) are at risk for sudden death. The contribution of arrhythmias is unclear. This study examines the prevalence of arrhythmias in children with the MFS and their relation to clinical and/or echocardiographic factors. Data from the Pediatric Heart Network randomized trial of atenolol versus losartan in MFS were analyzed (6 months to 25 years old, aortic root diameter z-score > 3.0, no previous aortic surgery and/or dissection). Baseline 24-hour ambulatory electrocardiographic monitoring was performed. Significant ventricular ectopy (VE) and supraventricular ectopy (SVE) were defined as ≥10 VE or SVE/hour, or the presence of high-grade ectopy. Three-year composite clinical outcome of death, aortic dissection, or aortic root replacement was analyzed. There were 274 analyzable monitors on unique patients from 11 centers. Twenty subjects (7%) had significant VE, 13 (5%) significant SVE; of these, 2 (1%) had both. None had sustained ventricular or supraventricular tachycardia. VE was independently associated with increasing number of major Ghent criteria (odds ratio [OR] = 2.13/each additional criterion, p = 0.03) and greater left ventricular end-diastolic dimension z-score (OR = 1.47/each 1 unit increase in z-score, p = 0.01). SVE was independently associated with greater aortic sinotubular junction diameter z-score (OR = 1.56/each 1 unit increase in z-score, p = 0.03). The composite clinical outcome (14 events) was not related to VE or SVE (p ≥ 0.3), but was independently related to heart rate variability (higher triangular index). In conclusion, in this cohort, VE and SVE were rare. VE was related to larger BSA-adjusted left ventricular size. Routine ambulatory electrocardiographic monitoring may be useful for risk stratification in select MFS patients.
Predictors of Rapid Aortic Root Dilation and Referral for Aortic Surgery in Marfan Syndrome.
Few data exist regarding predictors of rapid aortic root dilation and referral for aortic surgery in Marfan syndrome (MFS). To identify independent predictors of the rate of aortic root (AoR) dilation and referral for aortic surgery, we investigated the data from the Pediatric Heart Network randomized trial of atenolol versus losartan in young patients with MFS. Data were analyzed from the echocardiograms at 0, 12, 24, and 36 months read in the core laboratory of 608 trial subjects, aged 6 months to 25 years, who met original Ghent criteria and had an AoR z-score (AoRz) > 3. Repeated measures linear and logistic regressions were used to determine multivariable predictors of AoR dilation. Receiver operator characteristic curves were used to determine cut-points in AoR dilation predicting referral for aortic surgery. Multivariable analysis showed rapid AoR dilation as defined by change in AoRz/year > 90th percentile was associated with older age, higher sinotubular junction z-score, and atenolol use (R2 = 0.01) or by change in AoR diameter (AoRd)/year > 90th percentile with higher sinotubular junction z-score and non-white race (R2 = 0.02). Referral for aortic root surgery was associated with higher AoRd, higher ascending aorta z-score, and higher sinotubular junction diameter:ascending aorta diameter ratio (R2 = 0.17). Change in AoRz of 0.72 SD units/year had 42% sensitivity and 92% specificity and change in AoRd of 0.34 cm/year had 38% sensitivity and 95% specificity for predicting referral for aortic surgery. In this cohort of young patients with MFS, no new robust predictors of rapid AoR dilation or referral for aortic root surgery were identified. Further investigation may determine whether generalized proximal aortic dilation and effacement of the sinotubular junction will allow for better risk stratification. Rate of AoR dilation cut-points had high specificity, but low sensitivity for predicting referral for aortic surgery, limiting their clinical use.
Researchers studying the biology of the pediatric heart hope to help the next generation of children overcome heart disease. The following project is in development:
Electrical Stimulation of Pediatric Cardiac-Derived c-kit+ Progenitor Cells Improves Retention and
Cardiac Function in Right Ventricular Heart Failure
Principal investigator: Joshua T. Maxwell, PhD
Cardiac stem cells, otherwise known as progenitor cells, have shown promise in treating several problematic and sometimes lethal conditions like heart failure. Our HeRO investigators have been among the leaders in strategies to utilize these cardiac progenitor cells to reverse heart failure or to prevent it.
Dr. Maxwell and his colleagues employed a novel technique to enhance the efficacy of these cardiac progenitor cells, or CPCs, in a study published in Stem Cells. Leveraging early work from animal models, Maxwell’s team demonstrated that electrical stimulation of cardiac derived c-kit progenitor cells, taken from the pediatric patient at the time of newborn heart surgery, could improve the cardiac function and retention of the cells.
In well-designed experiments, Dr. Maxwell and his colleagues demonstrated the mechanism by which electrical stimulation improves CPC function. The impact of electrical stimulation can be seen in important clinical parameters in this model, including improved contractility of the right ventricle and lessened dilation of the right ventricle as a response to injury. Electrical stimulation of the CPCs also reduced fibrosis in the heart.
This work will support ongoing basic translational and clinical work in our Heart Center. We are currently undertaking a first-in-human trial of c-kit cardiac progenitor cells in hypoplastic left heart syndrome. The work of Dr. Maxwell and his colleagues has immediate applicability to these clinical trials and may impact direct patient care in the future.
Heart researchers are conducting clinical trials to discover new treatments and techniques in several areas of children’s heart care.
Visit clinicaltrials.gov to find a Children’s clinical trial. Search for “Children’s Healthcare of Atlanta” and your child’s condition.
Developing a Model to Predict Trial Outcomes for Babies with Hypoplastic Left Heart Syndrome
In 2020, clinicians and researchers from Children’s, University of Maryland Medical Center and University of Miami launched a novel trial that involved implanting patient-derived stem cells into the hearts of babies with hypoplastic left heart syndrome (HLHS) in an effort to strengthen the heart’s ability to pump blood. Now, a research team led by one of the leaders of that study, Michael Davis, PhD, Director of the Emory and Children’s Heart Research and Outcomes Center, is taking their investigation one step further.
Using patient genomic data from the CHILD study, the team has developed a computational model to try to predict what benefits may exist for a small subset of patients receiving the stem cell treatment. Babies born with HLHS do not have a functioning left side of the heart. There is a single ventricle doing the work of two ventricles. As a result, it is under a lot of stress and can fail. These babies require surgery shortly after birth, and will undergo three surgeries total over the course of three years, to redirect blood flow through the right side of the heart.
Dr. Davis and his team discovered that the cardiac-derived c-kit+ progenitor cells, or CPCs, which were injected into the babies’ hearts during the trial, were effective due to the release of what is known as extracellular vesicles, or nanoparticles, that play a critical role in intercellular communication.
Yet not all patients exhibited the same level of improvement. To identify contributing factors of cell therapy variability and improve clinical outcomes, the investigators took a machine learning approach by developing a collection of algorithms to attempt to establish patterns from the data and associate those patterns with definitive class samples. They combined the RNA sequencing of CPCs and their vesicles and cardiac-relevant cellular test tube experiments to build a predictive model.
They isolated CPCs from the cardiac biopsies of 29 patients with congenital heart disease and five patients with HLHS from the trial. The team then sequenced the cells and their vesicles and measured various responses from the vesicles.
They found the most important RNA signals involved in reparative outcomes had a significant link to cardiac development and signaling pathways. Furthermore, using a model trained on previously collected CPCs and their vesicles, they were able to predict outcomes for the trial’s clinical samples. Finally, they found that CPCs and their vesicles’ performance in building new blood cells correlated to clinical improvements in right ventricle performance. They published the results in iScience.
“This computational approach may pave the way for personalized medicine and predictive models for pediatric congenital heart disease therapy,” said Dr. Davis, Professor of Biomedical Engineering at Georgia Tech and Emory. “There were changes and we could detect them by sequencing the extracellular vesicles from the cells prior to injection.”
Placing Stem Cells Into the Hearts of Babies With Congenital Heart Disease
Principal investigator: Michael Davis, PhD, Director of the HeRO Center and Professor of Biomedical Engineering at Georgia Tech and Emory University
In this groundbreaking trial, surgeons at Children’s will implant patient-derived stem cells into the hearts of babies with hypoplastic left heart syndrome (HLHS) while they are undergoing surgical repair. The cells are collected during a baby’s first surgery within the first few days of life and then implanted into the heart three to five months later during the second of three HLHS surgeries. In the future, Dr. Davis and his research partners hope to gather quantitative data on the behavior of stem cells to create a large data repository of cell signals. By studying the signals, otherwise known as protein secretions of the cell, the team aims to determine how effective certain cells are in treating diseases.
COVID-19 and the heart
COVID-19 has significantly impacted children in Georgia, and researchers at Children’s are playing a critical role in understanding the cardiovascular impact of COVID-19. We are participating in two important national studies of COVID-19 and Multisystem Inflammatory Syndrome in Children (MIS-C) through two NIH studies, Pragmatic and Implementation Studies for the Management of Pain to Reduce Opioid Prescribing (PRISM) and MUSIC, An Observational Cohort Study to Determine Late Outcomes and Immunological Responses After Infection With SARS-CoV-2 in Children With and Without Multisystem Inflammatory Syndrome (MIS-C).
Long-Term Outcomes After the Multisystem Inflammatory Syndrome in Children (MIS-C) Study
Principal investigator: Matt Oster, MD, Pediatric Cardiologist
The goal of this research, conducted across 29 different sites as part of the Pediatric Heart Network, is to determine the spectrum and duration of coronary artery involvement, left ventricular (LV) systolic function, arrhythmias or conductions system disturbances within the first year from MIS-C illness onset, and to define the associated clinical and laboratory factors. Two published studies resulted from this work:
- Examination of Adverse Reactions After COVID-19 Vaccination Among Patients with a History of Multisystem Inflammatory Syndrome in Children
- Design and Rationale of the MUSIC Study
Catheterization lab
Comparison Between Surgical vs. Balloon Angioplasty vs. Intravascular Stent Placement for Recurrent or Native Coarctation of the Aorta
Principal investigator: Dennis Kim, MD, PhD, Pediatric Cardiologist
This study compares the safety and efficacy of three methods for treating coarctation, a narrowing of the aorta: surgical angioplasty, balloon angioplasty and stent placement. Angioplasty is a procedure that’s used to open arteries that are narrowed or blocked by plaque, a fatty buildup. It can be performed using a traditional open heart procedure or a catheter-based procedure—a minimally invasive technique that uses a thin, flexible tube inserted through a small incision and threaded to the blocked area. Balloon angioplasty has a small balloon on the tip of the catheter that’s inflated at the blockage to compress the plaque against the artery wall. A stent is a small, expandable tube that’s inserted into the artery during angioplasty to hold open the artery.
Cardiac Intensive Care
Gut Microbiome and its Association with Growth Trajectories in Infants with Congenital Heart Disease
Principal investigator: Michael Fundora, MD, Pediatric Cardiologist
This study examines if good bacteria influences growth and how it changes during the hospital course in babies with congenital heart disease. In partnership with Jinbing Bai, PhD, assistant professor at the Emory University School of Nursing and expert on the microbiome, Dr. Fundora will recruit 50 babies from the Children's Heart Center's cardiac intensive care unit (CICU) and 50 control babies from Emory Midtown, and match them to each other to compare their gut microbiome before and after surgery, and at discharge. The goal is to observe if there is disruption in the microbiome before and after surgery, how it changes during that period and determine its relationship to weight gain, head circumference and length, to see if there is any evidence the microbiome has an impact on growth. If so, future larger trials may lead to an interventions to promote weight gain after surgery which is associated with better outcomes. This research is funded by the Emory School of Medicine I3 Nexis award at $75,000 for two years.
Children’s Cardiologist Publishes COVID-19 Vaccination and Myocarditis Research
Dr. Matthew Oster, pediatric cardiologist at the Children’s Heart Center, led a descriptive study looking at data from the Vaccine Adverse Event Reporting System (VAERS) through the Centers for Disease Control and Prevention (CDC) to understand the risks and outcomes of myocarditis after mRNA-based COVID-19 vaccination through Moderna and Pfizer. Myocarditis is inflammation of the heart from viral infection. This data was collected across the U.S. from more than 190 million individuals ages 12 and up. From this population, there were 1,991 reports of myocarditis and 1,626 met the case definition for the condition. Findings showed that the risk of myocarditis after receiving mRNA-based COVID-19 vaccines was increased across multiple age and sex groups. Males made up 82% of cases, and rates of myocarditis were highest after the second vaccination dose in adolescent males ages 12-17 and young men ages 18-24. Of those with myocarditis who were hospitalized, 87% had resolution of presenting symptoms at hospital discharge. The study was published in JAMA on January 25, 2022.
Children’s Cardiologist Partners with Georgia Tech for IV Safety Study
Children’s cardiologist Zahidee (Saidie) Rodriguez, MD, partnered with Georgia Tech engineers to research a newly developed sensory device that significantly improves IV safety. This device helps nurses detect and reduce infiltration, which is unintended IV leakage that is common in children due to small vein size.
AMPK activator-treated human cardiac spheres enhance maturation and enable pathological modeling
Cardiac pathological outcome of metabolic remodeling is difficult to model using cardiomyocytes derived from human-induced pluripotent stem cells (hiPSC-CMs) due to low metabolic maturation.
There is a critical need for biomarkers of acute cellular rejection (ACR) in organ transplantation. We hypothesized that ACR leads to changes in donor-reactive T cell small extracellular vesicle (sEV) profiles in transplant recipient circulation that match the kinetics of alloreactive T cell activation. In rodent heart transplantation, circulating T cell sEV quantities (P < .0001) and their protein and mRNA cargoes showed time-specific expression of alloreactive and regulatory markers heralding early ACR in allogeneic transplant recipients but not in syngeneic transplant recipients. Next generation sequencing of their microRNA cargoes identified novel candidate biomarkers of ACR, which were validated by stem loop quantitative reverse transcription polymerase chain reaction (n = 10). Circulating T cell sEVs enriched from allogeneic transplant recipients mediated targeted cytotoxicity of donor cardiomyocytes by apoptosis assay (P < .0001). Translation of the concept and EV methodologies to clinical heart transplantation demonstrated similar upregulation of circulating T cell sEV profiles at time points of grade 2 ACR (n = 3 patients). Furthermore, T cell receptor sequencing of T cell sEV mRNA cargo demonstrated expression of T cell clones with intact complementarity determining region 3 signals. These data support the diagnostic potential of T cell sEVs as noninvasive biomarker of ACR and suggest their potential functional roles.
We conducted a phase 1 open-label multicentre trial to assess the safety and feasibility of Lomecel-B as an adjunct to second-stage HLHS surgical palliation. Lomecel-B, an investigational cell therapy consisting of allogeneic medicinal signalling cells (MSCs), was delivered via intramyocardial injections. The primary endpoint was safety, and measures of RV function for potential efficacy were obtained. Ten patients were treated. None experienced major adverse cardiac events. All were alive and transplant-free at 1-year post-treatment, and experienced growth comparable to healthy historical data. Cardiac magnetic resonance imaging (CMR) suggested improved tricuspid regurgitant fraction (TR RF) via qualitative rater assessment, and via significant quantitative improvements from baseline at 6 and 12 months post-treatment (P < 0.05). Global longitudinal strain (GLS) and RV ejection fraction (EF) showed no declines. To understand potential mechanisms of action, circulating exosomes from intramyocardially transplanted MSCs were examined. Computational modelling identified 54 MSC-specific exosome ribonucleic acids (RNAs) corresponding to changes in TR RF, including miR-215-3p, miR-374b-3p, and RNAs related to cell metabolism and MAPK signaling.
Bleeding is a serious complication of cardiopulmonary bypass (CPB) in neonates. Blood product transfusions are often needed to adequately restore hemostasis, but are associated with significant risks. Thus, neonates would benefit from other effective, and safe, hemostatic therapies. The use of fibrinogen concentrate (FC; RiaSTAP, CSL Behring, Marburg, Germany) is growing in popularity, but has not been adequately studied in neonates. Here, we characterize structural and degradation effects on the neonatal fibrin network when FC is added ex vivo to plasma obtained after CPB.
We’re widely recognized for our MRI studies of the heart and our heart echocardiography (ultrasound) program. Our dedicated core laboratory, the CIRC, is developing new strategies to evaluate the heart under conditions of stress or exercise.
Our researchers are working with colleagues at Georgia Tech to use imaging technology to create a 3D reconstruction of the heart. This will help us continue to improve the way we plan and carry out heart surgery in young patients.
The Cardiovascular Imaging Research Core (CIRC) lab was established in 2011 to conduct cardiac imaging research studies and incorporate novel and non-traditional imaging techniques into clinical practice. CIRC provides non-invasive cardiac imaging support for investigators engaged in clinical research involving fetuses, neonates, infants, children and adolescents. Our dedicated team of physicians, scientists, sonographers and research coordinators is experienced in utilizing cardiac imaging modalities and techniques not typically seen in the clinical setting.
The CIRC has dedicated laboratory space on both the Arthur M. Blank and Scottish Rite hospital campuses. It is one of only a few labs in the country with the infrastructure to provide support for pediatric cardiac imaging research. In addition to cardiology, CIRC services have been used by several other clinical services, including but not limited to cardiothoracic surgery, nephrology, hematology-oncology, neurology, genetics, gastroenterology and infectious diseases.
The CIRC is located at Children’s Healthcare of Atlanta at 2220 N Druid Hills Rd NE.
Please call 404-785-CIRC (2472) to access CIRC services.
Research services offered by CIRC include:
- Imaging protocol development
- Clinical site training and quality monitoring
- Image analysis
- Image transmission
- Data management
- Research quality imaging
- Cardiac MRI logistical and analysis support
Testing offered through CIRC includes:
- Echocardiography
- 2D, spectral and color Doppler
- 3D echocardiography
- Tissue Doppler imaging
- Strain and strain-rate imaging
- Vascular function assessment
- Cardiac computerized tomography including 3D reconstruction and digital printing
- Cardiac magnetic resonance imaging, including 4D flow
- Exercise stress testing
- Stress echocardiograms
- Electrocardiograms (EKG)
- Holter monitoring
Multicenter Core Lab Capabilities at CIRC
In 2016, CIRC created an infrastructure to serve as a multicenter core lab. Cardiac imaging studies from multiple centers can now be sent to CIRC for off-line analysis using a vendor-neutral software. Sites participating in the study upload images to our picture archiving and communication system (PACS) using a cloud-based technology. Our experienced team provides unbiased, centralized analysis of the deidentified images using a specialized software that minimizes errors that may result when images are collected from multiple centers using different imaging machines. CIRC staff maintains an electronic research database for the studies, as well as an image repository for all studies analyzed.
Collaborations
Our national research collaborations include:
- Pediatric Heart Network
- Fetal Heart Society
- Children’s Oncology Group
- Cardiac Genetics Registry
- FORCE (Fontan collaborative)
- American College of Cardiology Quality Network
- Society of Pediatric Echocardiography
Leadership
Ritu Sachdeva, MD, FACC, FASE, Medical Director
Researchers are exploring areas in which heart disease and neurological development impact one another. Our findings will help us develop new therapies to improve the quality of life for children with heart disease—everything from medications and traditional psychological therapy techniques to at-home strategies to help families.
Learning and social interaction
Research shows that a large percentage of children with congenital heart disease face academic challenges, including attention problems and difficulties planning and executing important daily tasks, known as executive function. In addition, there’s emerging evidence that these children may have problems interacting with their peers, which can have a serious impact in adolescence and young adulthood. Peer interaction is an important part of a child’s emotional development, including self-esteem and identity.
By evaluating children at 1 year old and again at 2 years old, we’re better able to understand the causes of these problems and develop therapies to improve outcomes.
Infant brain injury
Our researchers are analyzing infant brain injury and exploring the causes of the inflammatory process with MRI and the latest translational tools. In preliminary results, we’ve found that more than 50% of newborns who require open heart surgery have injury to the white matter in their brain. We’re exploring how signals within the body, called cytokines, may contribute to this process. Researchers need to gather more information to understand the factors that contribute to early brain injury, but this research could help us prevent it more effectively.
Patients with hypoplastic left heart syndrome who have been palliated with the Fontan procedure are at risk for adverse neurodevelopmental outcomes, lower quality of life, and reduced employability. We describe the methods (including quality assurance and quality control protocols) and challenges of a multi-center observational ancillary study, SVRIII (Single Ventricle Reconstruction Trial) Brain Connectome. Our original goal was to obtain advanced neuroimaging (Diffusion Tensor Imaging and Resting-BOLD) in 140 SVR III participants and 100 healthy controls for brain connectome analyses. Linear regression and mediation statistical methods will be used to analyze associations of brain connectome measures with neurocognitive measures and clinical risk factors. Initial recruitment challenges occurred that were related to difficulties with: (1) coordinating brain MRI for participants already undergoing extensive testing in the parent study, and (2) recruiting healthy control subjects. The COVID-19 pandemic negatively affected enrollment late in the study. Enrollment challenges were addressed by: (1) adding additional study sites, (2) increasing the frequency of meetings with site coordinators, and (3) developing additional healthy control recruitment strategies, including using research registries and advertising the study to community-based groups. Technical challenges that emerged early in the study were related to the acquisition, harmonization, and transfer of neuroimages. These hurdles were successfully overcome with protocol modifications and frequent site visits that involved human and synthetic phantoms.
Children with CHD show abnormalities in brain development before birth, but the neurological insults continue throughout development. All domains of ND and psychosocial functioning can show areas of weakness in CHD, but outcomes are variable. These ND concerns can span into adulthood leading to challenges with the adult transition. Thus, referral for ND evaluation is of paramount importance using the 2012 AHA guidelines for high-risk CHD.
More and more children with heart problems are living decades beyond what was expected in previous generations. But sometimes this success comes at a high price: neurological problems, lingering heart problems and damaged organs due to years of poor blood flow.
The Center for Cardiac Outcomes Research is exploring ways to meet the long-term needs of children with heart disease and their families.
Research goals are to:
- Determine what improves the quality of life for most children with heart disease.
- Prevent future complications related to a child’s heart condition.
- Use electronic medical records to do research and improve long-term follow-up care for these children.
Researchers are involved in dozens of projects that include public health policy, clinical review and technical innovation. One current project is evaluating whether all newborns should receive screening that can detect previously missed heart defects—whether the rare chance that the screening catches a defect justifies the additional cost of the test. This is an example of how studies measure both what’s medically effective and what’s cost effective.
In addition, the research team is exploring clinical practices to determine whether there are trends of consistently good long-term outcomes or if treatment at a certain point of children’s development results in better outcomes when they’re adults.
Procedure-Specific Center Volume and Mortality After Infantile Congenital Heart Surgery
Regionalization of congenital heart surgery (CHS) has been proposed to improve postsurgical outcomes by increasing experience in the care of high-risk patients. We sought to determine whether procedure-specific center volume was associated with mortality after infantile CHS up to 3 years post-procedure.
To evaluate the hypothesis that childhood survival for individuals with Down syndrome (DS) and congenital heart defects (CHDs) has improved in recent years, approaching the survival of those with DS without CHDs.
Children’s investigators have been addressing key topics in heart failure and heart transplantation.
Use of Ventricular Assist Device (VAD) to Support Patients Before Transplantation
Dr. Butto presented important work at the 2020 American Heart Association meeting that looks at the best approach to transplant listing after VAD implant. Her analysis of a large dataset found that it may be best to wait several weeks after a VAD is implanted before proceeding with a heart transplant in children. The likely explanation for this benefit is that the child can rehabilitate and enhance his nutritional status before receiving the transplant.
Principal investigator: Arene Butto, MD, Pediatric Heart Failure Physician
Dr. Butto presented important work at the 2020 American Heart Association meeting that looks at the best approach to transplant listing after VAD implant. Her analysis of a large dataset found that it may be best to wait several weeks after a VAD is implanted before proceeding with a heart transplant in children. The likely explanation for this benefit is that the child can rehabilitate and enhance his nutritional status before receiving the transplant.
Studying Heart Failure in Children and Young Adults With Congenital Heart Disease Using the Pediatric Care Consortium
Principal investigator: Lazaros Kochilas, MD, Pediatric Cardiologist
Dr. Kochilas and his team leveraged the large database, Pediatric Cardiac Care Consortium, housed at Children’s and Emory University, to understand how heart failure impacts children and young adults with CHD.
VALOR: VALOR A Phase 2/3 Randomized, Placebo-Controlled, Double-blind, Clinical Study to Evaluate the Efficacy, Safety, and Pharmacokinetics of Vericiguat in Pediatric Participants With Heart Failure Due to Systemic Left Ventricular Systolic Dysfunction (VALOR)
Pivotal PumpKIN: Pumps for Kids, Infants and Neonates (PumpKIN): The Jarvik 2015 Pivotal Trial (PumpKIN)
FCF and Heart Transplant: The Impact of Fontan Circulatory Failure on Heart Transplant Survival: A 20 Center Study
Our areas of interest include:
- Mechanical support of the failing heart
- Heart failure management
- Blood group incompatible transplants (donor and recipient don’t have compatible blood types)
- Noninvasive markers of transplant rejection
- Antibody-mediated rejection, which occurs when a transplant recipient’s own antibodies attack (reject) the new transplant
- Re-transplantation
- Paul J. Chai, MD, Chief of Cardiothoracic Surgery and Co-Chief of the Children’s Heart Center
- William T. Mahle, MD, Chief of Cardiology and Co-Chief of the Children’s Heart Center
- Michael Davis, PhD, FAHA, Director of Research
- Erin Buckley, PhD
- Michael Davis, PhD, FAHA
- Ilanit Itzhaki, PhD
- Lazaros Kochilas, MD
- Jennifer Q. Kwong, PhD
- Matthew Oster, MD, MPH
- Sung Jin Park, PhD
- Vahid Serpooshan, PhD
- Chunhui Xu, PhD

