At the Children's Heart Center, quality of care is our top priority. We closely monitor our surgical and non-surgical outcomes and volumes and make this data available so that parents have the most accurate information available as they choose the best hospital for their child's heart surgery.
Studies have shown that cardiac programs that perform a higher volume of heart surgeries may lead to better outcomes. These facilities typically have experienced heart surgeons who treat a variety of heart conditions, highly skilled staff and dedicated facilities to provide specialized postoperative care for heart patients.
As one of the largest pediatric cardiac programs in the country and the only nationally ranked pediatric cardiology and heart surgery program in Georgia*, the Children’s Heart Center:
- Performs more heart surgeries than anyone else in Georgia.**
- Performs some of the most complex procedures, with excellent outcomes.
- Is ranked top five in the nation for Cardiac Intensive Care Unit (CICU) and Cardiac Acute Care Unit Volumes (CACU).
- Is ranked in the top 5 in the nation for total pediatric heart transplant volumes since the program’s inception in 1988.***
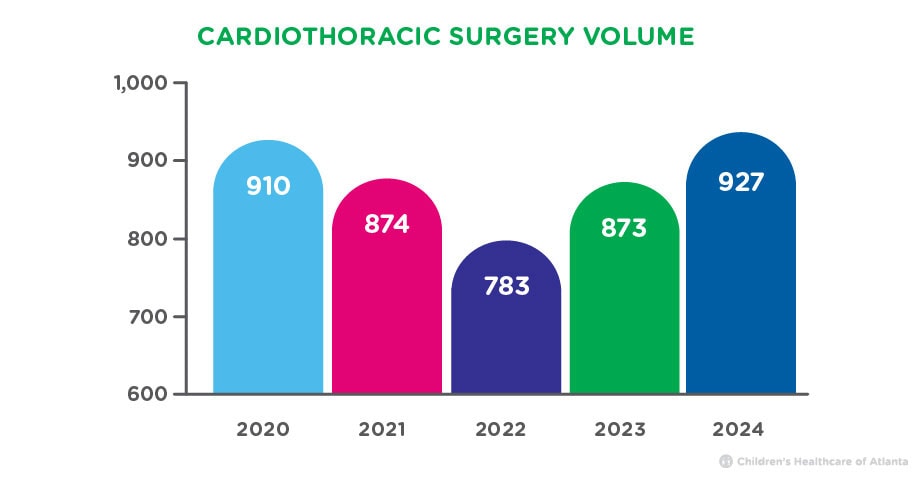
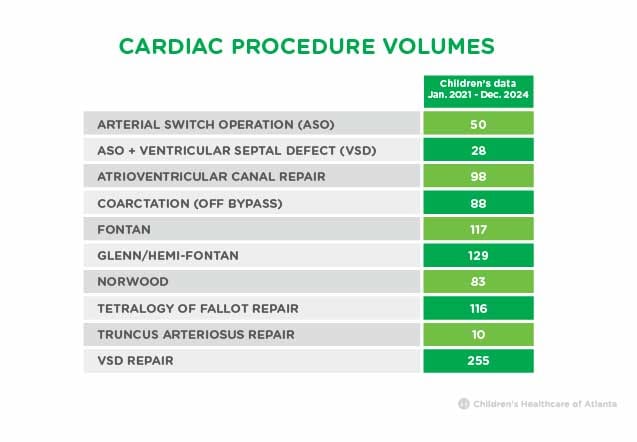
Cardiothoracic Surgery Case Volumes
Cardiothoracic surgery is any surgery related to or involving the organs in the chest, which includes heart surgery. The Children’s Heart Center performs hundreds of cardiothoracic surgeries each year.
 Catheterization Volumes
Catheterization Volumes
A heart catheterization is a nonsurgical procedure that can be used to diagnose heart defects, their location and severity. It can also be used to treat certain heart conditions without surgery. We offer a complete range of interventional catheterization procedures, including balloon valvuloplasty, angioplasty of vessels, stenting, atrial septal defect (ASD) and ventricular septal defect (VSD) occlusion and transcatheter pulmonary valve replacement. In 2024, our cardiac catheterization team performed 1,230 catheterization procedures.

Your Child's Heart Deserves Nationally Ranked Care
Children’s has the only nationally ranked cardiology and heart surgery program for kids and teens in Georgia.
learn moreHow We Compare Heart Surgery Outcomes
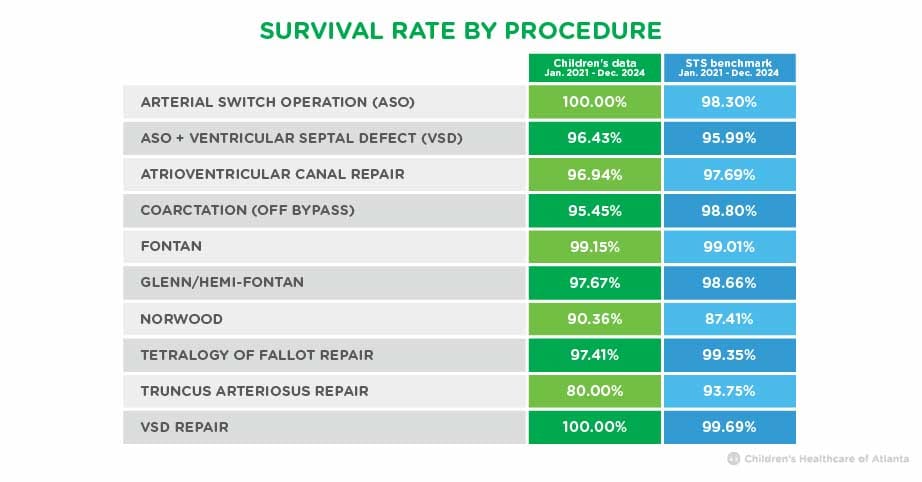
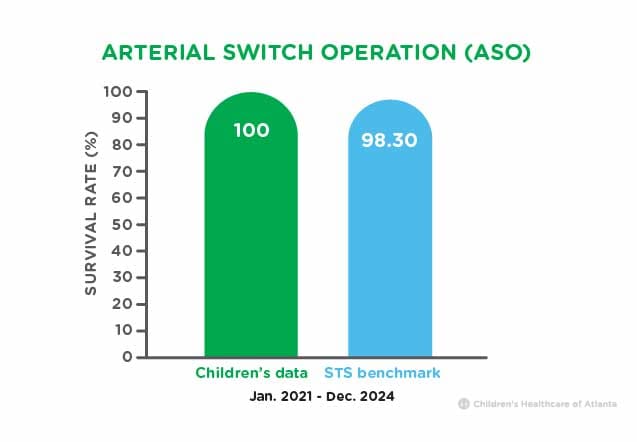
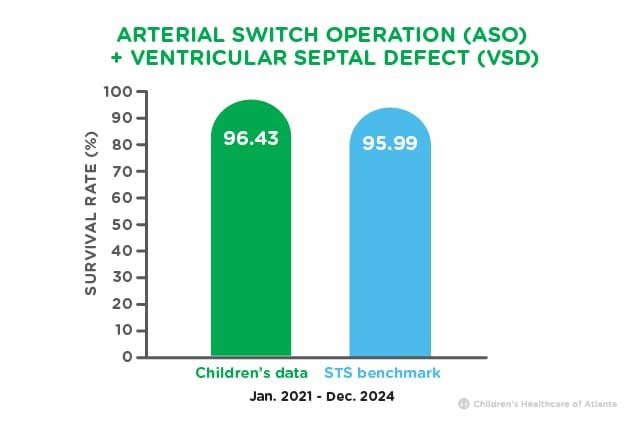
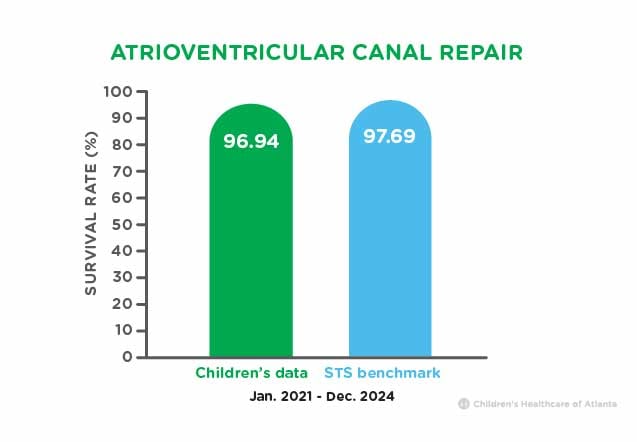
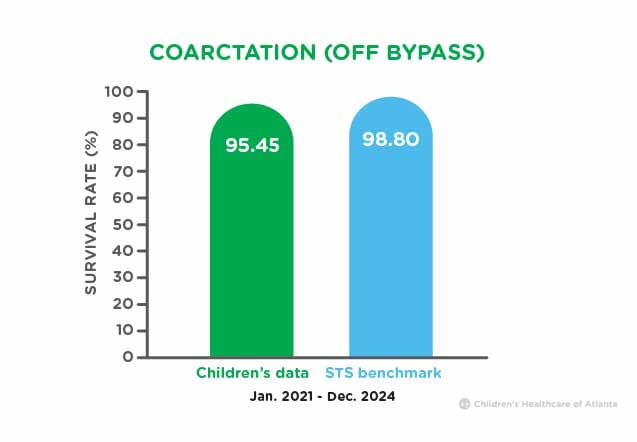
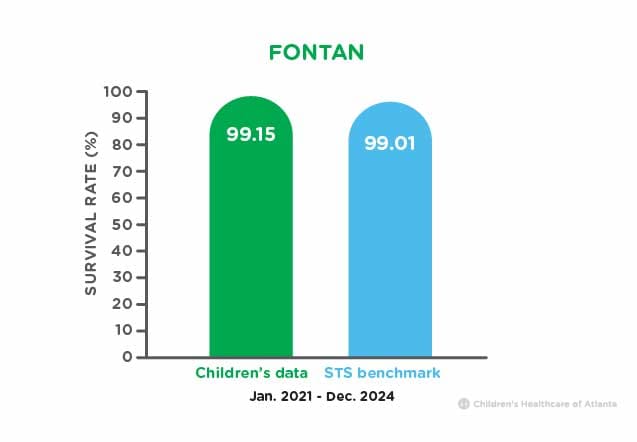
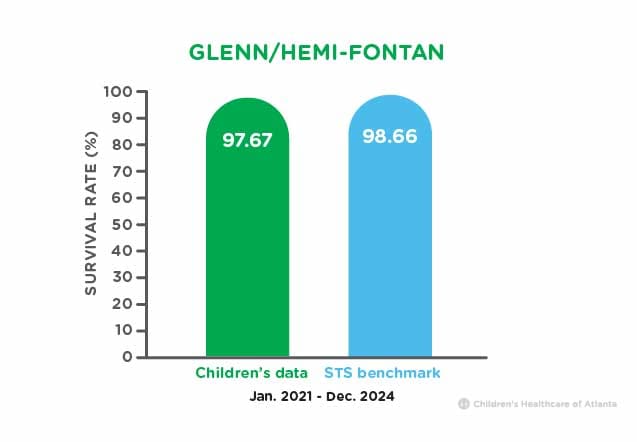
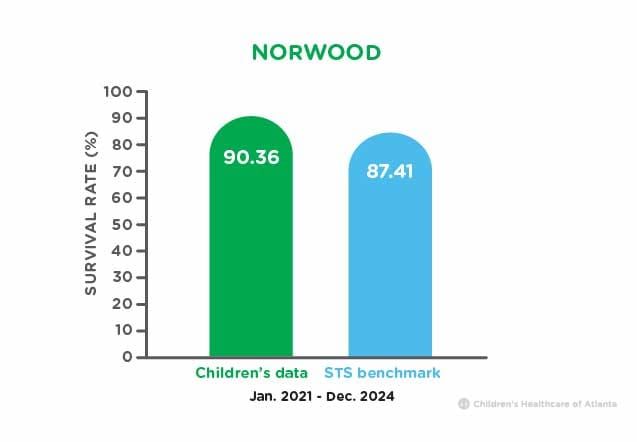
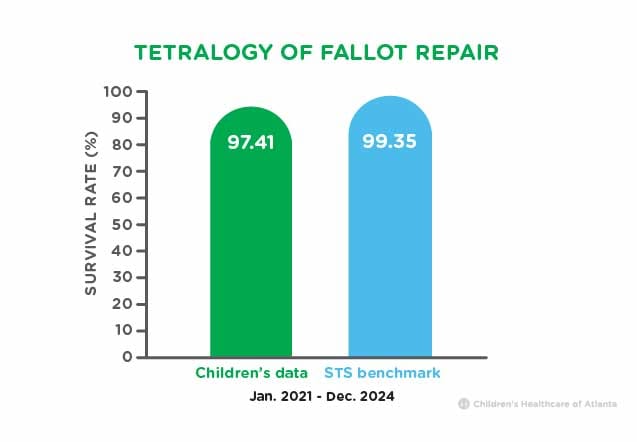
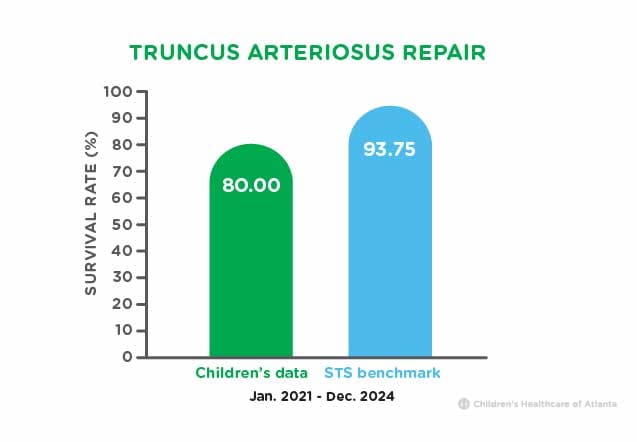
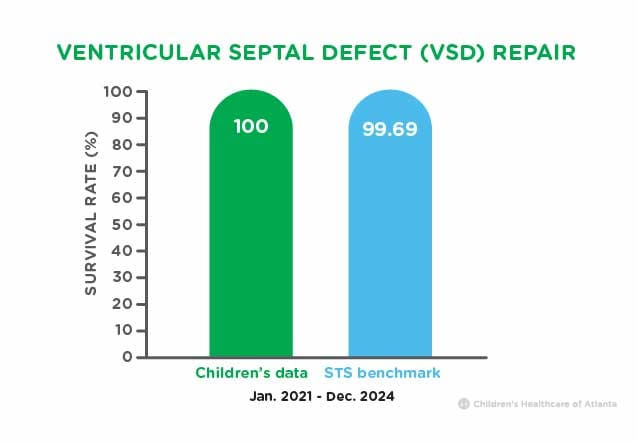
While the Children’s Heart Center performs many types of heart surgeries, there are 10 procedures called benchmark procedures that are used to compare the performance of surgical centers. The Society of Thoracic Surgeons (STS) collects and averages survival rates of these 10 procedures from facilities across the country to determine the national average, or STS benchmark. We monitor our surgical outcomes and compare them with the STS benchmark. Children's data (below) shows the number of benchmark procedures performed and their survival rates compared to the national average from January 2021 to December 2024.
This procedure is an open-heart surgery to correct transposition of the great arteries (TGA). During this surgery, the aorta and pulmonary artery are moved or switched back to the correct ventricle. The coronary arteries are also moved and attached back to the aorta. Children born with TGA will require life-long, follow-up care by a cardiologist.
In addition to moving the aorta and pulmonary artery back to the correct ventricle in the Arterial Switch Operation, the surgeon closes the ventricular septal defect (VSD), or hole, between the two lower chambers of the heart. The coronary arteries are also moved back onto the aorta. Children born with a TGA and VSD will require life-long, follow-up care by a cardiologist.
The surgery for atrioventricular canal (AVC) involves closing a large opening or hole that extends from the upper chambers (atria) to the lower chambers (ventricles) of the heart. An abnormal common valve is present and is rebuilt into the mitral and tricuspid valves. Children born with AVC will need life-long, follow-up care by a cardiologist.
To surgically correct the narrowing of the aorta, or coarctation, the surgeon enlarges the aorta to allow blood to flow freely to the lower part of the body. Children born with a coarctation will require life-long, follow-up care by a cardiologist.
This surgery is done as the last stage for patients born with a single ventricle, like HLHS. The surgeon connects the child’s inferior vena cava (IVC), a large vein from the lower body, directly to the lung artery to increase oxygen levels and decrease the amount of work placed on the heart. Children born with single ventricle will need life-long follow-up by a cardiologist.
This surgery is generally done as the second stage for patients born with a single ventricle, like HLHS, and occurs when the infant is 4 to 6 months old. The surgeon connects the child’s superior vena cava (SVC), a large vein from the upper body, directly to the lung artery. It allows the SVC to supply the lungs with blood and serves as a shunt, giving the child a few years to grow before the Fontan. Children born with a single ventricle will need life-long follow-up by a cardiologist.
This surgery is needed for patients born with a single ventricle , like HLHS . The Norwood procedure is usually done in the first week of life. A new or “neo” aorta is made from part of the pulmonary artery and the tiny aorta which is enlarged to provide blood flow to the body. A small tube graft is placed either from an artery coming off the aorta to the lung artery (called a modified Blalock-Taussig-Thomas shunt) or from the right ventricle to the lung artery (called a Sano shunt). Children born with a single ventricle will need life-long follow-up by a cardiologist.
This open heart surgery opens up blockage from the right pumping chamber of the heart and closes existing holes. Some infants require a temporary tube supplying blood to the lungs prior to surgery.
This congenital defect requires surgery to detach the pulmonary arteries from the common artery and connect them to the right ventricle using a valve-containing tube. A patch is used to close the ventricular septal defect.
Surgery is required to close a VSD, an abnormal opening between the two lower pumping chambers of the heart. The hole may be closed in a variety of ways depending on its size.
Children’s data shows the number of procedures performed from January 2021 to December 2024.
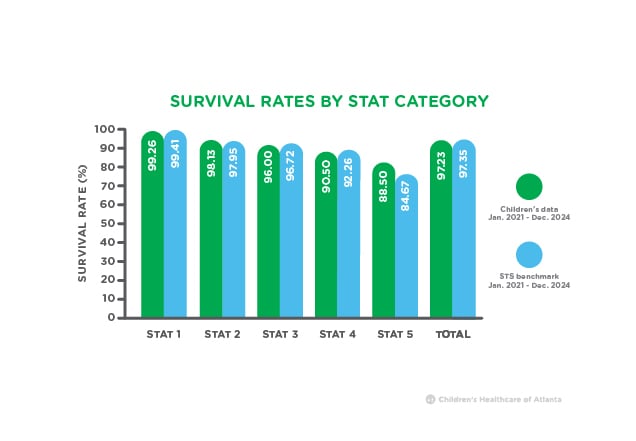
Survival Rate by Complexity
STAT category refers to a method of categorizing surgeries based on how risky or complex they are. STAT 1 surgeries have the lowest risk of death, while STAT 5 represents surgeries with the highest risk.
STAT 1: Patch repair of the atrial septal defect (ASD), ventricular septal defect (VSD) or pulmonary valve replacement
STAT 2: Ross procedure, Fontan procedure, tricuspid valve repair
STAT 3: Complete AV canal (AVC) repair, arterial switch operation (ASO)
STAT 4: Blalock-Taussig-Thomas (BTT) shunt, heart transplant, truncus arteriosus repair
STAT 5: Norwood procedure
Children's data is based on surgeries performed from January 2021 to December 2024.
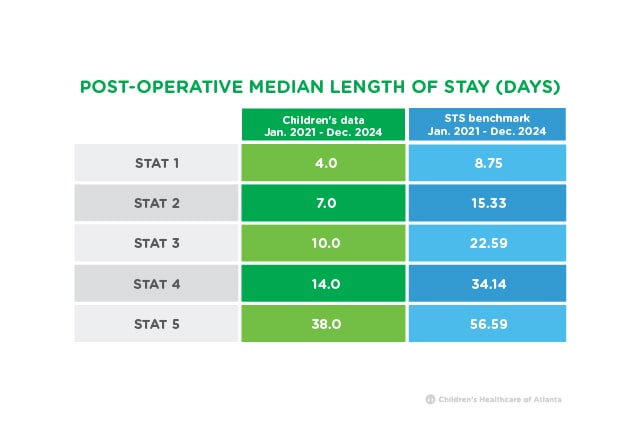
Length of Stay
Children’s Healthcare of Atlanta uses a process called Enhanced Recovery After Surgery (ERAS) to help reduce complications, better manage post-surgery pain and get kids home sooner. Our postoperative length of stay for heart surgeries is less than the national average.
Children's data is based on surgeries performed from January 2021 to December 2024. STS data is also based on surgeries performed from January 2021 to December 2024 as reported in the STS Congenital Heart Surgery Database Report.
The Scientific Registry of Transplant Recipients (SRTR) performs assessments of transplant outcomes every six months by looking at the outcomes of patients who underwent transplant over two and a half years.
The Scientific Registry of Transplant Recipients (SRTR) performs assessments of transplant outcomes every six months by looking at the outcomes of patients who underwent transplant over two and a half years.
For heart transplants that were performed at the Children’s Heart Center Jan. 1, 2022 to June 30, 2024, 89.67% of pediatric patients were alive with a functioning transplant one year after transplant, compared to a national average of 92.85%.
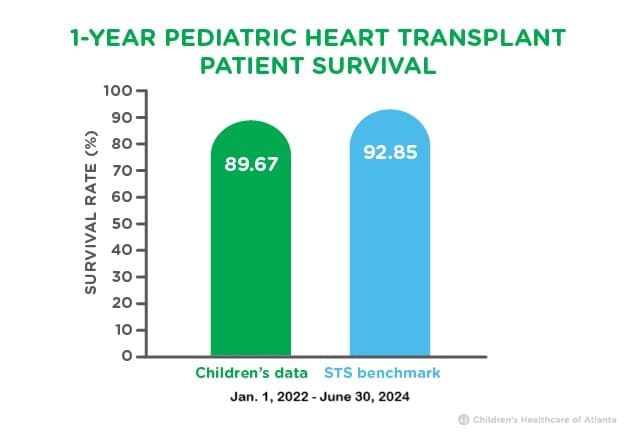
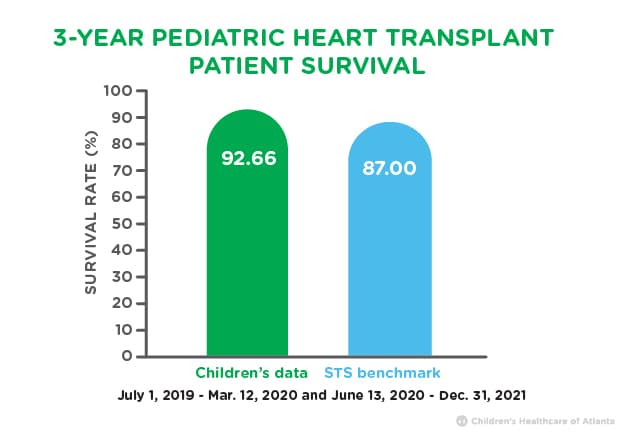
For heart transplants that were performed at the Children’s Heart Center between July 1, 2019 to Mar. 12, 2020 and June 13, 2020 to Dec. 31, 2021, 92.66% of pediatric patients were alive with a functioning transplant three years after transplant, compared to a national average of 87%.
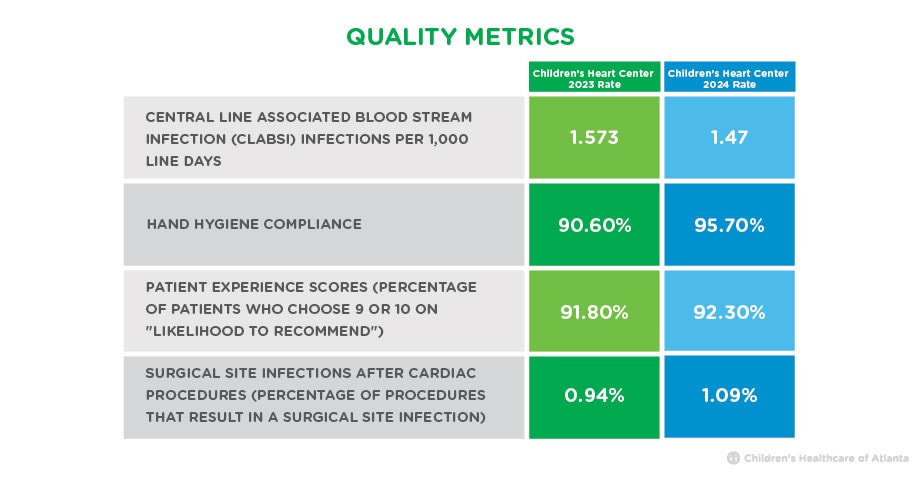
Children’s data (below) compares quality metric data from 2023 and 2024.
We publicly report our outcomes on our website and through U.S. News & World Report, the Society of Thoracic Surgeons (STS), the Scientific Registry of Transplant Recipients (SRTR) and the Conquering CHD Hospital Navigator. We also submit data to various clinical data registries and collaboratives, which allows us to compare ourselves to other pediatric heart centers to continuously improve the outcomes for our patients.
- Society of Thoracic Surgeons (STS) Congenital Heart Surgery Database for surgical outcomes. The STS has the largest congenital heart surgery database in the nation. Data from more than 100 hospitals is captured by STS to compare outcomes between heart programs across the country. We compare our outcomes to other STS pediatric heart surgery centers.
- Pediatric Cardiac Critical Care Consortium (PC4) data registry includes all medical and surgical patients admitted to a cardiac intensive care unit (CICU).
- Pediatric Acute Care Cardiology Collaborative (PAC3) data registry includes all patients in a cardiac acute care unit (CACU).
- National Pediatric Cardiology Quality Improvement Collaborative (NPC-QIC), which encompasses clinical process and outcomes data centered on the care of infants with single ventricle heart disease from prenatal diagnosis through their first year of life.
- Fontan Outcomes Network (FON) to measure outcomes of individuals with single ventricle disease.
- The Congenital Cardiac Catheterization Project on Outcomes (C3PO) is a data registry for pediatric CHD patients who undergo diagnostic catheterizations and catheter-based interventions.
- Clinical Cardiac Neurodevelopmental Outcome Collaborative (CNOC) clinical registry is a multicenter, multinational, collaborative data resource that works to optimize neurodevelopmental outcomes for individuals with pediatric and congenital heart disease.
- Pediatric Heart Transplant Society (PHTS) is an international prospective, event-driven database for children undergoing heart transplantation.
*No. 14 on the U.S. News & World Report “Best Children’s Hospitals” list for 2025-26.
**Georgia Hospital Association (GHA) by hospitals in Georgia, ages 0-18 (2022). Does not include any freestanding ambulatory surgery data.
***The Scientific Registry of Transplant Recipients (SRTR).
Contact Us 404-256-2593





