Arm and Elbow Injuries
Weekend Clinic for Injuries
Sprains, strains and broken bones don’t wait for weekdays. If your child needs to see a pediatric orthopedic expert on a weekend, Children’s has appointments available on Saturdays in Sandy Springs and Sundays in Duluth. Make an appointment online or call 404-255-1933 to schedule.
Make an AppointmentForearm fractures are typically the result of a fall and quite common in children of all ages. The forearm is made up of two bones: the radius (outside of the elbow) and ulna (long bone in the forearm). There are growth areas at the top and bottom ends of the forearm. The bottom growth areas near the wrist experience the most growth and are also more likely to be injured.
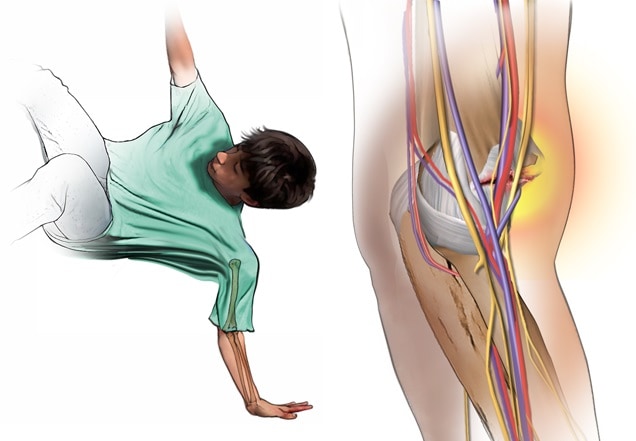
What is a Monteggia fracture?
A Monteggia fracture is a common arm injury that occurs when a child reaches out a hand to break a fall. The fracture is in the ulna, along with a dislocation of the radiocapitellar joint, which helps move the forearm. The force of the fall, paired with the fracture, forces the head of the radius to dislocate from the elbow joint.

How is a broken arm treated?
A simple forearm fracture is typically treated with a sling, ice and rest, but more complicated breaks may need a cast or surgery to help realign the broken bone. If a fracture moves within the cast into a position that can decrease future function, your child’s doctor may recommend surgery to place a temporary rod in either the radius or ulna. The rods stay inside the bone for approximately three to six months and are removed surgically.
Broken arms in older children and teens often require more than a cast for the following reasons:
- Older children have less growth left. The bones must heal straight to help make sure they can properly use their arms in the future.
- The lining around older bones is not as thick, which makes it easier for a broken bone to move around in the cast and not heal well.
- Older children have bigger, stronger muscles than younger children. Muscles are more likely to cause the fracture pieces to move around in the cast, disrupting healing.
Elbow injuries are common in children, however diagnosing an elbow injury in a young child can be difficult since a young child’s elbow joints are mainly cartilage, making injuries hard to spot on an X-ray. The elbow also has many growth centers that may be injured during a fall. These growth centers ossify (turn to bone) as a child grows and matures, making a child’s elbow X-rays at different ages look very different. Talk to your child’s doctor if you’re concerned about pain.
What if my child’s elbow is broken?
Elbow fractures are usually caused by a child falling while playing and injuring one of three bones: the humerus (upper arm bone), radius or ulna.
Elbow fractures often require surgery because:
- The fractured pieces are very separate from each other and would heal poorly if left in this position.
- The fracture crosses into the elbow joint and the bones need to be aligned as perfectly as possible to prevent future arthritis.
At Children’s Healthcare of Atlanta, our pediatric surgical experts are trained in treating elbow injuries in children from birth to age 18.
What are the different types of elbow injuries?
What is an elbow dislocation?
An elbow dislocation occurs when the joint between the ulna and humerus comes out of place. This injury:
- Accounts for roughly 3-6% of all pediatric elbow injuries.
- Happens three times as often to boys than girls.
- Is typically seen in children ages 10 to 15.
- Is extremely rare in children younger than age 3.
How is an elbow dislocation treated?
About half the time, the medial epicondyle is also fractured when the elbow dislocates. If there aren’t fractures with the dislocation, the joint is put back in place with your child under sedation, and the elbow is immobilized in a cast or splint for about a week. If there is a fracture in addition to the dislocation, surgery may be required.
Regaining range of motion is the biggest obstacle during recovery. Elbow dislocations associated with broken bones, especially in adolescent children, have the highest risk of developing stiffness later. Depending on the age of your child and the severity of the injury, your doctor may recommend physical therapy to help regain motion.

What is a lateral condyle elbow fracture?
A lateral condyle elbow fracture typically happens when a child breaks his fall with an outstretched hand, fracturing the outside edge of the elbow joint. It is the second most common elbow fracture in children ages 5 to 10, accounting for 17-20% of all pediatric elbow fractures.
How is a lateral condyle elbow fracture treated?
Since lateral condyle elbow fractures often involve the growth plate and elbow joint surface, they require surgery to heal properly. During surgery, an incision is made on the outside of the elbow. The fractured pieces are realigned and held in place with pins. A cast is then applied over the pins and remains in place for three to four weeks as your child’s fracture heals.

What is a medial epicondyle elbow fracture?
Like other fractures, a medial epicondyle elbow fracture typically occurs as a result of a fall on an outstretched hand. It affects the inside portion of the elbow and is often associated with an elbow dislocation. When these two injuries occur at once, a bone fragment can get trapped inside the elbow joint.
How is a medial epicondyle elbow fracture treated?
A medial epicondyle fracture may require surgery, especially if there is fragment entrapment in the joint. If surgery is required, the fragment is moved back into place and fixed with a screw or pin. If no surgery is required, your child will only need four to six weeks of immobilization in a splint or cast for a full recovery.
What is nursemaid’s elbow?
Nursemaid’s elbow is a common injury that is usually caused by a sudden pull on a child’s arm. It’s seen most often in young children ages 2 to 5, since children in this age range have looser ligaments. The injury happens when the radial head (outside of the elbow) is pulled out of the joint with the humerus, trapping one of the ligaments around the elbow.
After this injury, your child can usually bend his arm slightly at the elbow but probably won’t want to move it.
How is nursemaid’s elbow treated?
Nursemaid’s elbow is easily corrected by a simple maneuver by a clinician, and your child can begin using his elbow normally within a few minutes. No further treatment is needed.
What is a radial head and neck elbow fracture?
A radial head and neck fracture is a break at the top of the radius just below the elbow joint. This type of fracture accounts for 1-5% of elbow injuries in children and usually occurs in children 9 to 10 years old.
How is a radial head and neck elbow fracture treated?
When this injury happens, the top of the radius needs to be put back into place, which can usually be done in an emergency department with your child under sedation. The elbow will then be immobilized in a splint or cast for approximately one week.
What is a supracondylar humerus fracture?
A supracondylar humerus fracture is a break to the humerus just above the elbow joint in an area of thin, weak bone called the supracondylar region. It can damage the nerves, blood vessels and muscles surrounding the elbow. This type of fracture accounts for more than half of the fractures around the elbow. It’s most common in children 5 to 7 years old, since parts of their elbow are still thin and developing. Symptoms may include severe pain, swelling and inability to move the elbow.
How is a supracondylar elbow fracture treated?
Supracondylar fractures need to be evaluated as soon as possible by a pediatric-trained orthopedist who can check for damage in the blood vessels, nerves and muscles, as well as compartment syndrome. Compartment syndrome happens when there is not enough blood supply to a body part after an injury. It can lead to further muscle and nerve damage.
Treatment for a supracondylar elbow fracture depends on its severity. Many of these fractures are minimally displaced, meaning the bone pieces are relatively close together. If that is the case, we will immobilize the arm with a cast or splint for several weeks.
If the bones are separated far apart and appear crooked on X-rays, your child may need surgery to help align the bones and maintain position. Most of the time, no incision will be necessary to realign the bones. Instead, your surgeon will hold the bones in place with two to three sterile metal pins that are placed through the skin, inside the bone and across the fracture. The pins stay outside the skin but are protected underneath a cast. After three to four weeks of healing, the cast and pins will be removed. Once the pins are removed, your child may be placed back in a cast for a few weeks.

What is Little League elbow?
Little League elbow is an overuse injury caused by repeated throwing without enough rest between throws. During overhead throwing, the cartilage growth plate is placed under stress and becomes irritated, causing pain. The pain may be severe and can occur after one hard throw or gradually over a season. There may also be swelling, redness or warmth on the injured elbow.
What is osteochondritis dissecans?
Osteochondritis dissecans (OCD) is a joint condition in which the bone—in this case the elbow—underneath the cartilage of a joint dies due to lack of blood flow. OCD is a painful condition that occurs when lack of blood flow causes bone and cartilage to separate from the surface of a joint. The exact cause is unknown, but family history and repetitive trauma are thought to play a role. While OCD can occur suddenly with a specific traumatic event (such as a fall), it usually develops over time due to repetitive stress on the joint. OCD lesions are most often seen in active children over age 10—especially baseball pitchers, quarterbacks, gymnasts and swimmers. The repetitive motions associated with these activities exert compressive forces across the lateral (outside) part of the elbow. The first symptom is activity-related elbow pain in the dominant arm. Later symptoms may include catching, locking, grinding and loss of motion. It also happens in people whose bones are not straight.
How is osteochondritis dissecans of the elbow treated?
To diagnose OCD, your child will first undergo a physical exam, and the doctor will ask about any sports or activities he plays. The doctor may also recommend an X-ray or MRI.
The goal of OCD treatment is to restore normal joint function, decrease pain and reduce the risk of future osteoarthritis in the joint. About 90% of the time, resting the joint is all it takes. But every child is different. OCD treatments may include:
- Complete rest and no weight bearing at all to avoid any motion that may cause pain. Then, light daily life activities and weight bearing, as tolerated, can be introduced slowly.
- Casting, splinting or bracing the joint to keep it still.
- Avoiding sports and other intense activities.
- Sports physical therapy, which can be very effective in eliminating pain, preventing further injury and helping with flexibility and strength.
- Surgery:
- If there is no improvement after rest and physical sports therapy.
- If a piece of the bone breaks away completely.
- To fix a problem that may be causing OCD.
Once symptoms are gone and X-rays show the joint is healing, athletes may be ready to slowly progress back to their sports. This is best monitored by a physical therapist.
This content is general information and is not specific medical advice. Always consult with a doctor or healthcare provider if you have any questions or concerns about the health of a child. In case of an urgent concern or emergency, call 911 or go to the nearest emergency department right away. Some physicians and affiliated healthcare professionals on the Children’s Healthcare of Atlanta team are independent providers and are not our employees.
Contact Us 404-255-1933